
What are health care providers to do if they are in short supply of the swabs to perform COVID-19 tests?
A test requiring a specimen is only as good as the quality of that specimen collected. As test kits accessibility is improving, providers are now finding shortages of other supplies required to do the test for COVID-19. In addition to PPE shortages there is now a swab shortage! Should we be taking a specimen from another site?
What makes this difficult as there is very little data demonstrating what the ideal specimen may be with COVID-19. There is some limited data mostly from the experience of China that has conflicting information. We understand this virus is acting differently than other viruses we typically test for such as influenza and RSV. Its clinical symptom presentation is different and has turned into a more virulent lower respiratory pathogen. At this critical time the CDC and health systems are evaluating their option. Should they be considered using a different type a swab or a different location such as sputum or oropharynx?
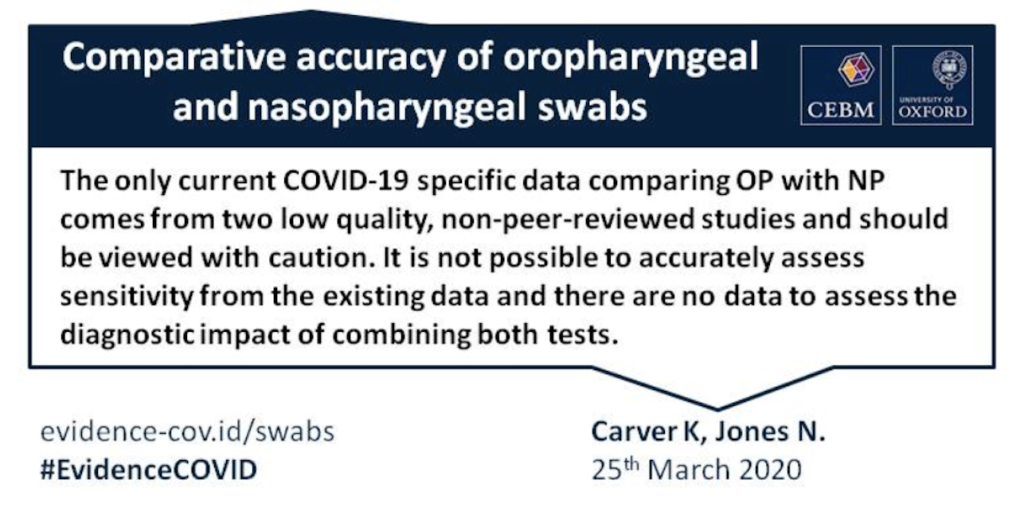
The CDC has adapted its recommendations based on the above difficulties over the last several weeks. Upon reviewing their guidelines it seems they will take whatever they can get??? Until we have better statistical significant analysis, we must base our decisions on what is has been proven previously.
What is proven?
A nasopharyngeal swab is deemed a less expensive and an advocated method for specimen collection. However, the science and statistical analysis tells us that nasopharyngeal aspirate (NPA) is actually the better of the two. All historical studies demonstrate the superiority of sensitivities of a nasopharyngeal aspirate over a nasopharyngeal swab including influenza and RSV. In ideal laboratory situations studies have demonstrated a nasopharyngeal swab can approach the sensitivities of nasopharyngeal aspirate. None of these studies ever exceed the sensitivities of NPA. NPA is the gold standard! NP swab sensitivities are less than ideal as nurses and medical assistants are poorly trained in proper technique. We are now asking them to test while patients are sitting in the drivers seat of car. To complicate it further they are now performing a nasopharyngeal swab with their left hand. Is there anyone else wondering how drive thru testing sensitivities compare to other techniques?
So why are we not performing nasopharyngeal aspirates?
Typically providers are unaware how to properly perform or are unaware of the proper equipment required to perform a NPA. Certainly a swab is cheaper, easier and possibly more convenient. However a swab has a higher false negative rate and is typically performed incorrectly. The swab most times is never getting to the nasopharynx because of poor technique and associated patient discomfort. Why not use a Nasopharyngeal Kit making it easier for everyone? A properly performed nasopharyngeal aspirate is more comfortable for the patient and results in a better specimen result. A properly perform nasopharyngeal aspirate with a syringe and catheter can also be less irritating to the patient. This causes less cough and sneezing than a poorly performed irritative swab thereby reducing risk for aerosolization. This is VERY important for a highly contagious pathogen such as COVID-19.
Looking for the most historically sensitive means of specimen collection for COVID-19 with the least amount of discomfort and aerosolization? No swab!?!?
Start performing nasopharyngeal aspirations for Covid-19!
- Click here for our instructional video on how to properly perform a nasopharyngeal aspiration.
- Look for our next blog on how to properly perform a NP swab!

